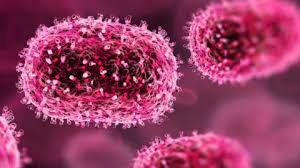
Scabies
People are being told not to ignore an itchy rash, with GPs in England reporting a spike in scabies - the highly infectious skin infestation.
The condition is caused by a mite which burrows under the skin to lay eggs and is spread through close physical contact, bedding and clothes.
It can spread quickly in places where people live closely together, such as universities and care homes, the Royal College of GPs (RCGP) said.
'Tiny red dots'
Some 3,689 cases were diagnosed in hospitals in England in the year to April – up from 2,128 the previous year, according to NHS figures.
The BBC has heard from people at five universities around the country, who spoke of multiple cases arising "out of nowhere" and whole houses having scabies.
One student said BBC "tiny red dots" along his wrist had begun spreading.
"One of my housemates came out to the house that she had scabies at the time as well. So then I was like, 'Okay, so do I'," he added.
More on this story
Another student told us he had been trying to get rid of it for "two to three months". When we asked how he thought he had caught it he said: "Probably a lot of sleeping together”.
Prof Hawthorne said: "We recognise that patients may be apprehensive to seek treatment given the social stigma that surrounds the condition, but it is important that they don’t ignore their symptoms as this could lead to them getting worse and risks transmitting the condition to other people."
Everyone infected needs to be treated at the same time with a cream or lotion from the pharmacy, doctors say.
Patients are also advised to wash their bedding and clothes on a high temperature.
Dr Alison George, a GP in the north of England who works in an emergency department, said many students come straight to A&E, but only after the disease has become worse.
"It can be really nasty. It is then really difficult to treat if you've got a really large area of the body covered in it."
Some 3,689 cases were diagnosed in hospitals in England in the year to April – up from 2,128 the previous year, according to NHS figures.
The BBC has heard from people at five universities around the country, who spoke of multiple cases arising "out of nowhere" and whole houses having scabies.
One student said BBC "tiny red dots" along his wrist had begun spreading.
"One of my housemates came out to the house that she had scabies at the time as well. So then I was like, 'Okay, so do I'," he added.
Another student told us he had been trying to get rid of it for "two to three months". When we asked how he thought he had caught it he said: "Probably a lot of sleeping together”.
Prof Hawthorne said: "We recognise that patients may be apprehensive to seek treatment given the social stigma that surrounds the condition, but it is important that they don’t ignore their symptoms as this could lead to them getting worse and risks transmitting the condition to other people."
Everyone infected needs to be treated at the same time with a cream or lotion from the pharmacy, doctors say.
Patients are also advised to wash their bedding and clothes on a high temperature.
Dr Alison George, a GP in the north of England who works in an emergency department, said many students come straight to A&E, but only after the disease has become worse.
"It can be really nasty. It is then really difficult to treat if you've got a really large area of the body covered in it."
#InfectiousDiseases, #ICID2024, or relevant year, #GlobalHealth, #DiseasePrevention, #InfectiousDiseaseConference, #PublicHealth, #Epidemiology, #DiseaseControl, #HealthInnovation, #VaccinationMatters, #PandemicPreparedness, #PathogenResearch, #OneHealth, #InfectionPrevention, #GlobalDiseaseOutbreak, #ViralResearch, #EmergingInfectiousDiseases, #HealthSecurity, #MedicalConference, #ICIDSummit
Visit Our Website : infectious-diseases-conferences.pencis.com
Nomination Link : infectious-diseases-conferences.pencis.com/award-nomination
Registration Link : infectious-diseases-conferences.pencis.com/award-registration
Member Link : infectious-diseases-conferences.pencis.com/conference-membership
Awards-Winners : infectious-diseases-conferences.pencis.com/awards-winners/
Contact us : infectious@pencis.com
Get Connected Here:
==================
Social Media Link
Twitter : twitter.com/skyla00827177
Blog : infectious2021.blogspot.com
Instagram : www.instagram.com/infectious_diseases2021
Facebook : www.facebook.com/pencis.queen
YouTube : www.youtube.com/channel
Wikipedia : infectiousdiseases625904580.wordpress.com